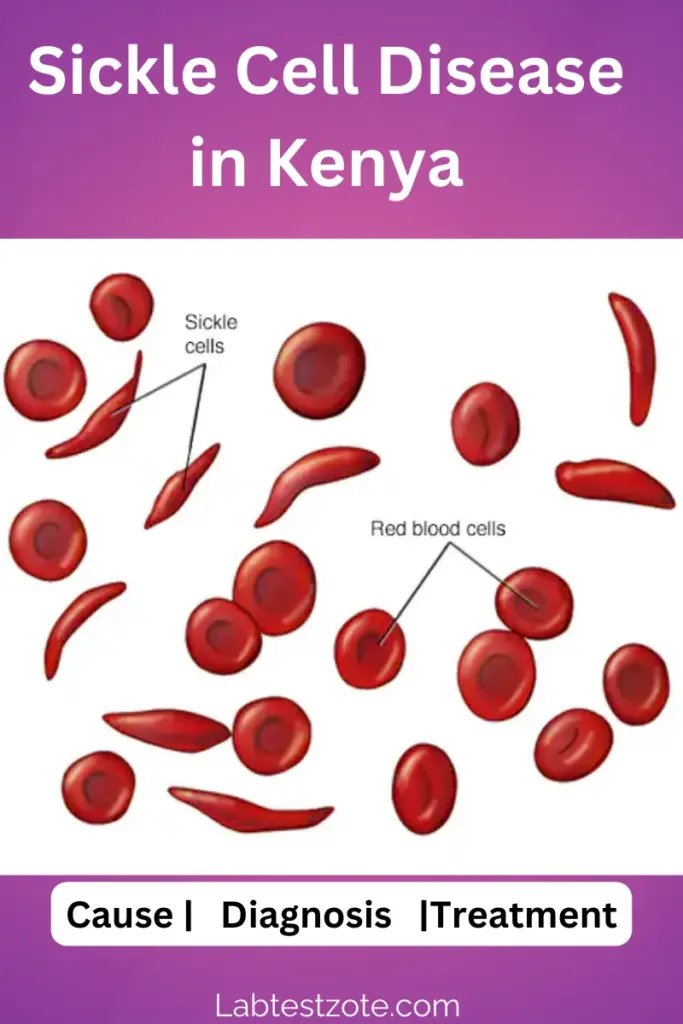
Sickle cell disease (SCD) is a serious genetic condition that affects red blood cells. These cells take on a sickle shape, causing them to get stuck in small blood vessels, leading to pain, infections, and organ damage.
In Kenya, SCD is a significant public health concern, with a high prevalence in certain regions. This comprehensive guide will explore SCD in Kenya, its impact, management options, and how to live well with the disease.
Understanding Sickle Cell Disease in Kenya
High-Risk Areas:
SCD is more prevalent in areas that historically overlapped with the malaria belt in Kenya. This includes Western Kenya (former Western and Nyanza provinces) and the Coast region. The reason for this link is complex, but it’s believed that the sickle cell trait offered some protection against malaria. However, with declining malaria rates, SCD has become a more prominent health concern. Additionally, due to migration patterns, SCD is also present in urban areas.
Genetic Inheritance:
SCD is an inherited disease passed down from parents, in autosomal recessive pattern. If both parents carry the sickle cell trait, there’s a 25% chance their child will have SCD.
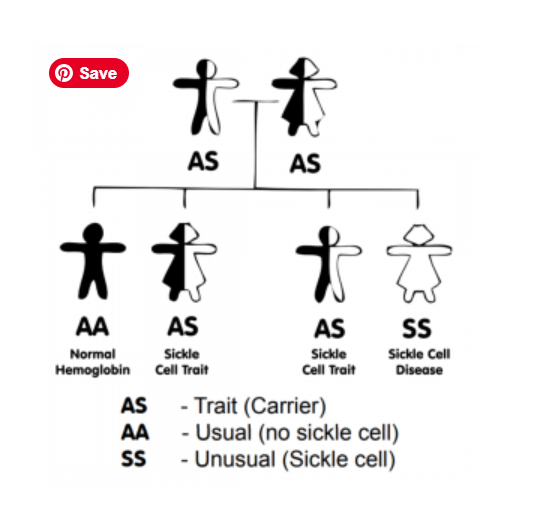
It’s important to understand the difference between SCD and the sickle cell trait (SCT). People with SCT carry only one abnormal sickle gene and typically don’t experience symptoms. However, they can pass the trait on to their children.
Impact of Sickle Cell Disease in Kenya
Burden on Children:
A significant number of children in Kenya are born with SCD each year. Without early diagnosis and intervention, children with SCD face a high mortality rate. This puts a tremendous strain on families and healthcare systems.
Challenges in Diagnosis:
Diagnosing SCD in Kenya can be challenging because some symptoms, like pain and fever, overlap with other common childhood illnesses such as malaria, pneumonia and meningitis. Early and accurate diagnosis is crucial for better management of the disease. Newborn screening programs play a vital role in achieving this.
Role of Laboratory in Diagnosis and Management of Sickle Cell Disease
We have emphasised the importance of early diagnosis. In this section, we will cover the role of laboratory tests in the management of this condition. These in include;-
- Sickle cell Trait Screening
- Newborn screening for sickle cell disease
- Confirmatory Tests for Sickle Cell Disease
- Sickle Cell crises and disease monitoring
Sickle Cell Trait Screening in Kenya
Sickle cell trait is the presence of one abnormal sickle cell gene. Since the person has a normally functioning gene, they typically have enough of the normal haemoglobin and do not show any of the symptoms of sickle cell disease
However, if two sickle cell trait individuals have a child, there is a 25% chance of getting a child with sickle cell disease.
The laboratory tests used to diagnose sickle cell trait (SCT) include:
- Sickle cell solubility test
The test involves adding an agent, such as sodium dithionite, to the blood sample, which causes the haemoglobin to release from the red blood cells and dissolve in the plasma5. If HbS is present, it will not dissolve easily in the plasma, causing the solution to become cloudy or turbid5.
The sickle cell solubility test is a quick and inexpensive screening test that can be used to identify individuals with sickle cell trait (SCT) or sickle cell disease (SCD)4,5.
- Hemoglobin Electrophoresis
This test separates the different types of haemoglobin based on their electrical charge. It is commonly used for screening and confirmation of SCT
- High-Performance Liquid Chromatography (HPLC
HPLC is a technique used to separate, identify, and quantify each component in a mixture of haemoglobin. It is an effective method for diagnosing SCT and other abnormal hemoglobinopathies[1][4].
d) DNA Testing
DNA testing can be used to identify specific genetic mutations associated with SCT. This method is particularly useful for confirming the presence of the sickle cell gene and determining carrier status[1].
These tests are essential for accurately diagnosing SCT and differentiating it from other abnormal hemoglobinopathies. They are crucial in informing genetic counselling, especially in high-prevalence regions like Kenya.
Newborn Screening for Sickle Cell Disease
In Kenya, the laboratory techniques used in newborn screening for sickle cell disease (SCD) include:
1. Haemoglobin electrophoresis
This is a laboratory technique used to analyse the different types of haemoglobin in red blood cells, including sickle cell disease (SCD)[1][2]. This test helps diagnose serious conditions like SCD and is one of several tests that screen newborn babies for SCD and other rare but serious illnesses[1].
The test involves applying an electric current to a blood sample, which separates normal and abnormal types of haemoglobin. Each type of haemoglobin can then be measured individually[2]. Normal types of haemoglobin include:
-
-
- Hemoglobin (Hgb) A, the most common type of haemoglobin in healthy adults
- Hemoglobin (Hgb) F, fetal haemoglobin, found in unborn babies and newborn
- Hemoglobin (Hgb) S, found in sickle cell disease
-
2. Isoelectric Focusing (IEF)
This technique is used to screen for hemoglobinopathies, including SCD and sickle cell trait (SCT)[2]. Laboratory personnel are trained on using the IEF technique to identify abnormal haemoglobin patterns in newborns[2].
2. High-Performance Liquid Chromatography (HPLC)
It is a more advanced and accurate method compared to IEF, making it a potential tool for use in Kenya’s newborn screening program.
3. Point-of-Care Tests (POC)
A portable and quick-reporting test system for SCD and SCT, such as the Sickle SCAN test developed by BioMedomics, has been approved for use in Kenya[1]. This test can accurately detect SCD and SCT in just five minutes, using only one drop of whole blood from the patient[1]. POC tests like Sickle SCAN could be a valuable addition to Kenya’s newborn screening program, as they offer a cost-effective and easy-to-use method for diagnosing both SCD and SCT without the need for external equipment, power source, or trained lab technicians[1].
Importance of Early Diagnosis:
Early diagnosis of SCD allows for better management and can significantly improve the quality of life for patients. Newborn screening programs are crucial for early detection and intervention.
Treatment Options for Sickle Cell Disease
There is currently no cure for SCD in Kenya. However, several treatment options can help manage the disease and improve patients’ well-being. These include:
- Pain Management: Effective pain management strategies are essential for people with SCD, as painful crises are a hallmark symptom.
- Hydration: Staying well-hydrated helps prevent complications and improve blood flow.
- Hydroxyurea: This medication can help reduce the frequency and severity of painful crises in some patients.
Healthcare providers play a critical role in educating patients and families about SCD management, treatment options, and the importance of adherence to medication regimens.
The Role of Advocacy and Support Groups
Advocacy groups and support networks play a vital role in raising awareness about SCD, providing support to patients and families, and advocating for improved access to healthcare services and resources.
Living with Sickle Cell Disease in Kenya
Living with SCD can be challenging, but with proper support and management, people with SCD can lead fulfilling lives. Here are some key aspects:
- Coping Mechanisms for Patients and Families: Learning about SCD, developing coping mechanisms for pain management, and connecting with support groups are crucial for patients and families.
- Importance of Genetic Counseling: Genetic counselling can help individuals and families understand the risks of passing SCD to future generations and make informed reproductive decisions.
- Future Advancements in SCD Treatment: Research into gene therapy and other novel treatment options offers hope for a potential cure for SCD in the future.
Conclusion
Sickle cell disease is a serious health concern in Kenya. However, with increased awareness, improved screening programs, comprehensive management strategies, and ongoing research, the future for people living with SCD in Kenya is brighter.
Disclaimer
The information provided on this medical blog is for general informational purposes only and should not be considered as a substitute for professional medical advice. Always consult with a qualified healthcare provider before making any healthcare decisions or taking any actions based on the information provided on this blog. The authors and publishers of this blog are not liable for any errors or omissions in the content or for any actions taken based on the information provided.
Leukemia (Blood Cancer) – Signs & Symptoms, Diagnosis and Treatment
Introduction to leukemia Leukemia, a form of blood cancer, arises in the bone marrow, causing…
How to Know Your ABO Blood Group and Why it Can Save Your Life
What are Blood Groups? A blood group is a way to categorize the type of…

